The Darzi report – a response.

We at the PCC were really interested in the recent publication of Lord Darzi’s Independent
Investigation of the NHS in England , and what its content might signify for the future of the
NHS, and therefore for our primary care teams.
This ‘diagnostic’ review feels refreshing in that it doesn’t avoid calling out difficult issues,
warts and all. Lord Darzi doesn’t only reflect on the state of the NHS; he also considers how
the nation’s deteriorating health impacts healthcare provision, and what he refers to as “a
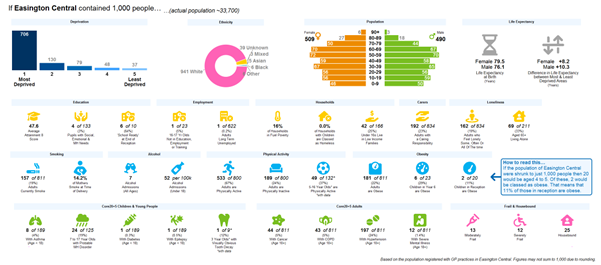
society in distress.” This recognition of the wider determinants of health (for example,
poverty, poor housing, lack of employment) is particularly resonant for us in the North East
and North Cumbria, where life expectancy at birth has been persistently lower than the
England average for a long time. The acknowledgement of the value of our healthcare
teams, and of listening to patients share their experiences is also very welcome.
Many of the problems will be well recognised, but we are not necessarily used to seeing
them called out nationally and clearly. A&E in an “awful state,” contracts with perverse
incentives not fit for purpose, declining public health budgets, too many regulators, national
guidance arriving late, single year contracts, performance standards that only reflect hospital care etc. The list goes on… This doesn’t make for positive reading, but it is honest.
There is an encouraging theme for primary care running through the report. Lord Darzi is
clear that GPs are doing more with less; more patients, more complexity, more appointments with fewer GPs and comparatively less funding.
The potential for community pharmacies to contribute more is also highlighted, and there is an understanding that dentists and optometrists are constrained by their contracts and struggling to keep going. The recommendation is that funding needs to be channeled into care closer to home, namely primary care and community services. Although this has been a strategy for many years, nonetheless the diagnosis has revealed that “left shift became right drift”, and funding went into hospital-based care. Lord Darzi feels that ICBs are sensible structures with a good chance of being able to tackle some of these issues.
The report is comprehensive (165 pages!) and for many people will contain no surprises,
although it is useful as a whole system overview. It is the next steps that will be key. What
are the proposed solutions? How can we help to shape them? Reading through the long list
of organisations who contributed to the study, it is difficult to find primary care represented. It will be vital for groups like our Primary Care Collaborative to be heard as we work together to improve, and, as always, we are keen to hear your thoughts.